WHAT IS
RELAPSING MS?
The more you know about relapsing forms of multiple sclerosis, the greater understanding you’ll have about how to manage therapy to fit your life. Get started by educating yourself on these key topics of the disease:
What is MS?1-3
Multiple sclerosis (MS) is most commonly known as a disease that affects the central nervous system (CNS), but 2 systems are involved in MS—the CNS and the immune system.
The nervous system has 2 main parts:
-
The central nervous system (CNS) is made up of the brain and spinal cord.
-
The peripheral nervous system (PNS) is made up of nerves that branch off from the spinal cord and extend to all parts of the body.
Neurons, or nerve cells, send signals through the CNS to other parts of the body along nerve fibers called axons. These signals control physical functions like balance and muscle coordination, as well as memory and other cognitive abilities.
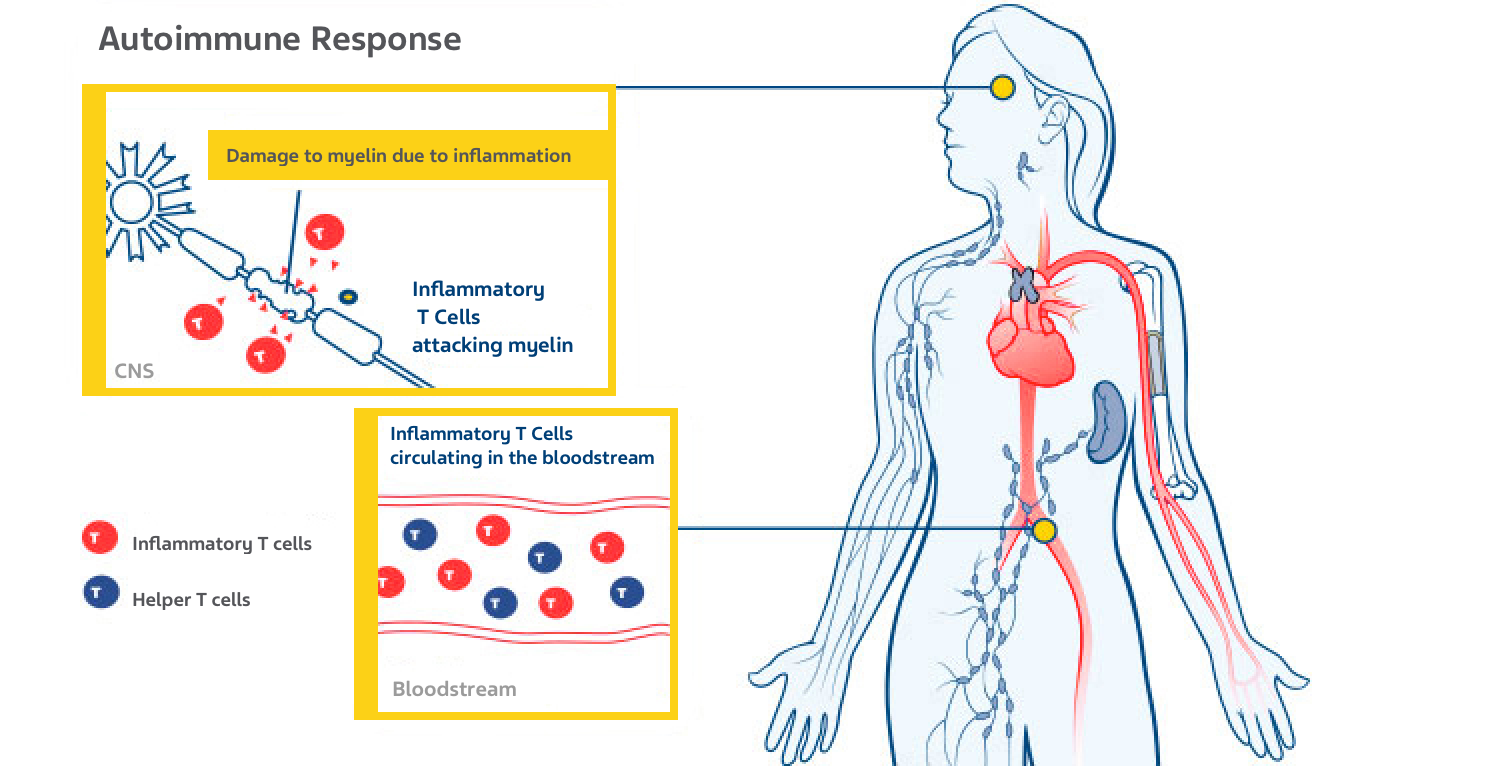
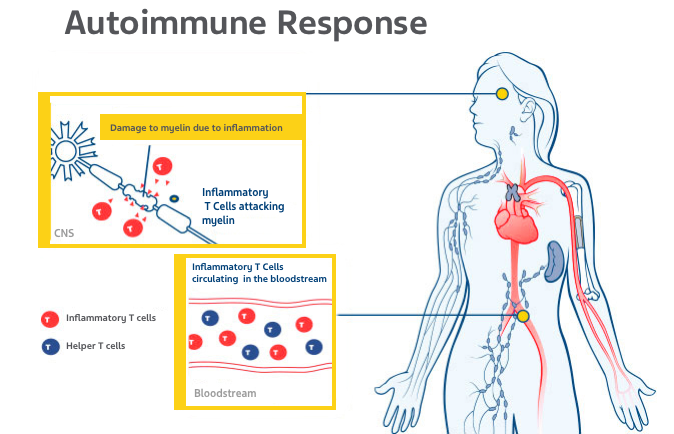
The immune system consists of unique types of cells such as T cells and B cells and proteins designed to identify and destroy infectious organisms and other invaders and incorrectly functioning cells.
What causes MS?1,4-7
Currently, the exact cause of MS is unknown. Inflammatory T cells attack the myelin that protects the axons, or nerve tissue, in the CNS. This results in scar tissue called scleroses (lesions) and disrupts the body’s ability to send signals from one part of the CNS to another, causing MS symptoms.
WHAT ARE THE EARLY SIGNS OF MS?5,8
Because MS affects 2 major systems within the body, it can manifest in multiple ways, but the 2 most common early symptoms are:
-
Optic nerve inflammation (optic neuritis) often starts with pain in the eye, headache on one side, or blurred vision.
-
Spinal cord inflammation (partial transverse myelitis) can appear as limb weakness, bowel and bladder issues, tingling, and numbness.
WHAT CAN TRIGGER MS RELAPSES?9-12
Most people with MS have what is called relapsing-remitting type, where they have relapses, then a remission where the symptoms either improve, stop getting worse, or go away entirely.
MS relapse occurs when inflammation of the nerves and myelin causes a temporary recurrence of existing symptoms or entirely new symptoms.
Pseudo-exacerbation can sometimes look like a relapse due to temporary worsening of MS symptoms, but there is no myelin inflammation occurring and it is often brought on by things like:
-
Increased body temperature—often due to an infection (urinary tract infection is the most common trigger), exercise, or hot weather
-
Mood changes—stress, depression, or exhaustion
WHAT IS THE PROGNOSIS FOR MS?13

Significant physical disability occurs within 20-25 years of the first appearance of symptoms in roughly one-third of people with untreated MS. Research has shown that several MS treatments can slow this progression; long-lasting benefits are unknown.
WHAT IS RELAPSING-REMITTING MULTIPLE SCLEROSIS (RRMS)?9,14
A person diagnosed with MS has damage in at least 2 separate areas of the CNS which occurred at different points in time and all other possible diagnoses have been ruled out.
RRMS is the most common form of MS, affecting approximately 85% of people with MS. Two or more attacks (relapses), are usually followed by partial or complete recovery. During remissions, there is no progression of disease and all symptoms may disappear.
WHAT ARE THE SYMPTOMS OF RELAPSING-REMITTING MULTIPLE SCLEROSIS (RRMS)?4,5,15,16
MS symptoms are highly individual, just like MS patients. They are unpredictable and vary from one person to another. The symptoms you may experience vary, depending on the location and the extent of the damage in your central nervous system. You may find that you experience some of the symptoms at different times during the course of MS. Even pregnancy can impact your symptom frequency. The most common MS symptoms are:
-
weakness
-
fatigue
-
numbness or tingling
-
walking (gait) difficulties
-
spasticity
-
dizziness
-
vision problems
-
bladder problems
-
bowel problems
-
depression
-
memory loss
-
difficulty concentrating
To learn more about MS symptoms, download our MS & Symptom Management Guide.
WHAT ARE THE TYPES OF MS?17-19
People diagnosed with clinically isolated syndrome (CIS) may experience only 1 attack, or event, of MS-like symptoms and may have brain lesions consistent with MS. Clinical studies have shown that treatment following a diagnosis of CIS can delay a second attack, thereby delaying the diagnosis of clinically definite relapsing MS. Starting treatment at an early stage and continuing treatment with an approved relapsing MS therapy can reduce relapses and may help reduce future damage from the outset.
WHAT ARE THE RISK FACTORS OF MS?20-22
Based on the worldwide distribution of MS, scientists have identified factors that may provide clues to the possible causes of MS. These include the following:
-
Gender: Women are 2 to 3 times more likely to have MS than men.
-
Genetics: MS is not directly inherited; however, the risk of getting MS rises in people who have a close relative (parent, sibling, or child) with MS.
-
Age: Most people are diagnosed with MS between the ages of 20 and 50.
-
Ethnic background: MS affects most ethnic groups, but it is more common among people of northern European ancestry.
-
Geography: MS occurs more frequently in people who live farther from the equator. Worldwide, more than 2.3 million individuals may be affected.
WHEN SHOULD I SEEK TREATMENT FOR RELAPSING MS?4,23,24
According to the National Multiple Sclerosis Society (NMSS):
Your doctor may consider starting treatment with an approved therapy as soon as possible after a diagnosis of relapsing MS, or after a first attack with magnetic resonance imaging (MRI) findings consistent with MS, and other possible causes have been ruled out. Although there is no cure for MS, COPAXONE® has been shown to help manage the disease.
References:
-
What is an immune-mediated disease? National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/Definition-of-MS/Immune-mediated-disease
-
What are the parts of the nervous system? Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). Accessed July 13, 2021. https://www.nichd.nih.gov/health/topics/neuro/conditioninfo/parts
-
Brain anatomy and how the brain works. Johns Hopkins. Accessed July 13, 2021. https://www.hopkinsmedicine.org/health/conditions-and-diseases/anatomy-of-the-brain
-
Multiple sclerosis. Mayo Clinic. Accessed July 13, 2021. https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
-
Definition of MS. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/Definition-of-MS
-
What is MS? Multiple Sclerosis Alliance of Southern Colorado. Accessed July 13, 2021. https://msasoco.org/who-we-are/what-is-ms.html
-
Multiple sclerosis: frequently asked questions. Cleveland Clinic. Accessed July 13, 2021. https://my.clevelandclinic.org/health/articles/14315-multiple-sclerosis-frequently-asked-questions
-
Rush Stories: early signs of multiple sclerosis. Rush University System for Health. Accessed July 13, 2021. https://www.rush.edu/news/early-signs-multiple-sclerosis
-
Relapsing-remitting MS (RRMS). National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org//What-is-MS/Types-of-MS/Relapsing-remitting-MS
-
Multiple sclerosis relapses. Multiple Sclerosis Association of America. Accessed July 13, 2021. https://mymsaa.org/ms-information/overview/relapses
-
Exacerbation. Pittsburgh Institute for Multiple Sclerosis Care and Research. Accessed July 13, 2021. http://www.ms.pitt.edu/diseasemanagement/exacerbation
-
Multiple sclerosis. Medline Plus. Accessed July 13, 2021. https://medlineplus.gov/genetics/condition/multiple-sclerosis/
-
Luzzio C. Multiple sclerosis. Medscape. Updated January 3, 2022. Accessed July 13, 2021. https://emedicine.medscape.com/article/1146199-overview
-
Diagnosing MS. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/Symptoms-Diagnosis/Diagnosing-MS
-
Pregnancy and reproductive issues. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/Living-Well-With-MS/Diet-Exercise-Healthy-Behaviors/Womens-Health/Pregnancy
-
MS signs and symptoms. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/Symptoms-Diagnosis/MS-Symptoms
-
Clinically isolated syndrome (CIS). National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/Types-of-MS/Clinically-Isolated-Syndrome-(CIS)
-
Treatments of CIS. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/Types-of-MS/Clinically-Isolated-Syndrome-(CIS)/Treatments
-
Clinically isolated syndrome (CIS). Multiple Sclerosis Trust. Updated February 2020. Accessed July 13, 2021. https://mstrust.org.uk/a-z/clinically-isolated-syndrome-cis
-
Who gets multiple sclerosis? Epidemiology of MS. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/Who-Gets-MS
-
What causes MS? National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/What-Causes-MS
-
Understanding MS. National Multiple Sclerosis Society (NMSS). Accessed July 13, 2021. https://www.nationalmssociety.org/What-is-MS/MS-FAQ-s#question-What-is-multiple-sclerosis
-
Costello K, Halper J, Kalb R, Skutnik L, Rapp R. The Use of Disease-Modifying Therapies in Multiple Sclerosis: Principles and Current Evidence. National Multiple Sclerosis Society (NMSS); 2014. Updated September 2019. Accessed July 13, 2021. https://www.nationalmssociety.org/getmedia/1e64b96c-9e55-400e-9a64-0cdf5e2d60fe/summaryDMTpaper-_final
-
COPAXONE® (glatiramer acetate injection) Current Prescribing Information Parsippany, NJ. Teva Neuroscience, Inc.
You are about to leave COPAXONE.com and enter a website operated by a third party.
Would you like to continue?
The information on this site is intended for healthcare professionals in the United States. Are you a healthcare professional in the United States?


